In one market access workshop, a payer representative once said to a biotech team, “Your data are excellent. They just don’t answer any of our questions.” The silence that followed summed up a familiar problem: great science, misaligned evidence.
The gap between clinical evidence and payer expectations remains one of the most expensive mistakes in drug development. It’s not that companies ignore value; they define it differently. Regulators focus on safety and efficacy, while payers focus on relative benefit, durability, and affordability. Bridging those two perspectives is the essence of evidence strategy.
Evidence Is Strategy, Not Administration
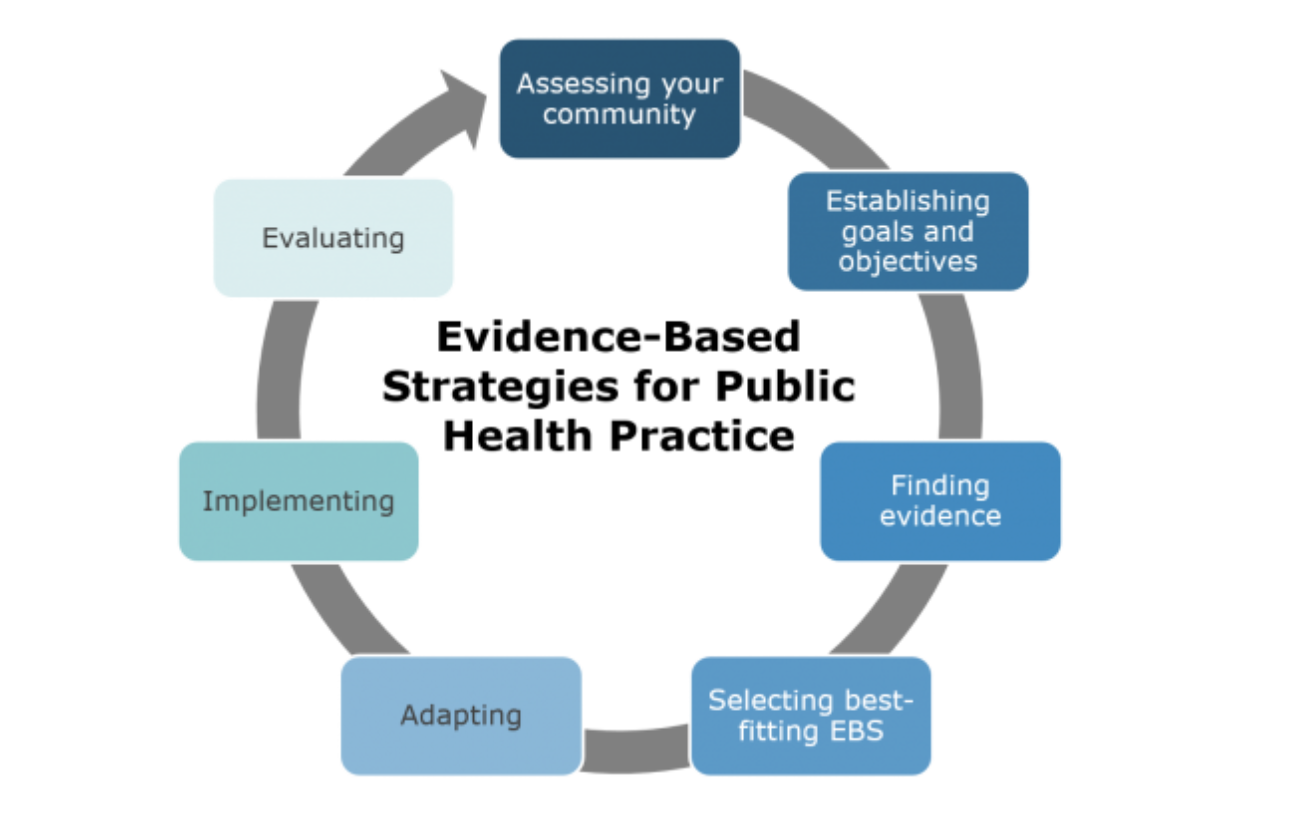
Many organisations still treat evidence planning as a technical task — a sequence of studies, endpoints, and reports. But evidence is strategic storytelling. It determines whether your product is seen as indispensable or irrelevant. The goal is not just to prove the drug works, but to prove that it changes the system meaningfully.
Early alignment between R&D, access, and health economics is vital. The most successful companies embed payer insight from the first protocol draft. They test assumptions about comparators, relevance of endpoints, and cost implications before the first patient is enrolled. This integration saves years later.
From Data to Demonstration
Evidence generation must move beyond volume to purpose. The question is no longer “Do we have enough data?” but “Do we have the right data for each stakeholder?” Regulators, clinicians, payers, and patients each interpret value differently.
In oncology, for example, progression-free survival might satisfy regulators but not payers, who need long-term quality-of-life and resource data. In chronic disease, patient adherence and functional outcomes often carry more weight than biomarker shifts. Knowing which lens each audience uses allows you to design studies that translate effectively across systems.
The Power of Real-World Evidence
Randomised trials remain the gold standard, but real-world evidence (RWE) now completes the story. It contextualises trial results in actual practice, showing durability, adherence, and equity of access. For payers, this evidence often determines long-term reimbursement stability.
The challenge is rigour. Poorly designed RWE can undermine confidence faster than no data at all. Standardised frameworks, validated endpoints, and transparent methodologies are essential. RWE should not be an afterthought; it should be a continuation of clinical strategy.
Anticipating Value Objections
The best evidence strategies anticipate resistance. Before submission, map every potential challenge a payer might raise — comparators, subpopulation data, affordability — and prepare corresponding evidence. Value recognition depends as much on preparation as on data.
This approach also improves internal alignment. When everyone understands what questions need to be answered, resources are allocated efficiently, and messages stay consistent.
The Bottom Line
Evidence is the currency of access, and strategy determines its exchange rate. Companies that excel at early, integrated evidence planning will change how value is recognised, not just shorten time to market.
Good science opens doors. Strategic evidence keeps them open.
Key Takeaways
- Evidence strategy is strategic communication, not paperwork.
- Alignment between R&D and access must begin early.
- Real-world evidence validates long-term value.
- Anticipating payer objections strengthens positioning.
- Data without context rarely translates into access.
Try This
Before your next evidence review, ask: “Does this dataset answer payer questions, or just regulatory ones?” If not, redesign it. Better to fix gaps in planning than in reimbursement.
Closing Thought
Share this with your medical or evidence generation colleagues. Value recognition comes faster from a clear purpose rather than data.